Know the Hazards of Uncontrolled Diabetes
High blood sugar levels can seriously damage parts of your body, including your feet and your eyes. These are called diabetes complications. But you can take action to prevent or delay many of these side effects of diabetes.

Over time, having too much glucose in your blood can cause complications,including: Eye disease, due to changes in fluid levels, swelling in the tissues, and damage to the blood vessels in the eyes. This can cause diabetic retinopathy (blur vision), diabetic macular edema (swelling), cataracts, and glaucoma. Over time, diabetes can cause damage to your eyes that can lead to poor vision or even blindness.
Foot problems, caused by damage to the nerves and reduced blood flow to your feet, this can lead to Loss of hair on your toes, feet, and lower legs. Dry, cracked skin on your feet.A change in the color and temperature of your feet. Thickened, yellow toenails. Fungus infections such as athlete’s foot between your toes. A blister, sore, ulcer, infected corn, or ingrown toenail.
Nerve problems (diabetic neuropathy), caused by damage to the nerves and the small blood vessels that nourish your nerves with oxygen and nutrients. This can cause the development of motor as well as sensory symptom.
Motor neuropathy symptoms
Nerve damage can lead to problems such as muscles weakness, which could cause falls or problems with doing tasks like fastening buttons, and muscles wasting where muscle tissues is lost because it’s less active. It can also lead to muscle twitching and cramps.
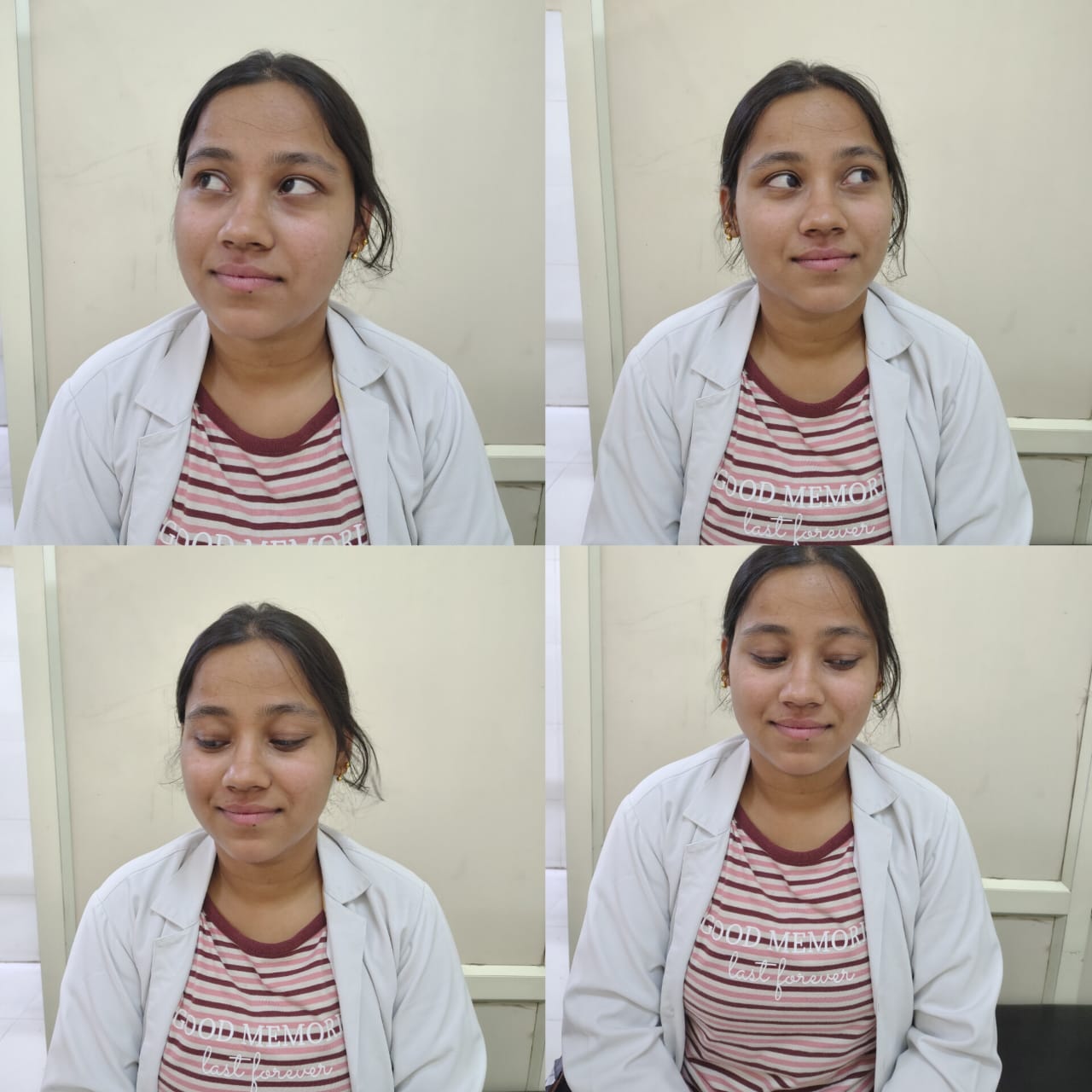
Symptoms of sensory neuropathy in feet, legs, hands and arms
1- tingling and numbness
2- loss of ability to feel pain
3- loss of ability to feel changes in temperature
4- loss of coordination – when you can’t feel the position of your joints
5- burning or shooting pains – these may be worse at night
Gum disease and other dental problems, because a high amount of blood sugar in your saliva helps harmful bacteria grow in your mouth. Other types cause tooth decay and cavities.
Heart disease and stroke, caused by damage to your blood vessels and the nerves that control your heart and blood vessels.
Kidney disease, due to damage to the blood vessels in your kidneys. Many people with diabetes develop high blood pressure. That can also damage your kidneys.
Sexual and bladder problems, caused by damage to the nerves and reduced blood flow in the genitals and bladder. Diabetes also causes excessive urination.
Skin conditions, People with diabetes are also more likely to have infections, including skin infections.
Musculoskeletal problems, Diabetes is associated with a number of musculoskeletal disorders including adhesive capsulitis of the shoulder, tenosynovitis of the long flexor of the fingers and thumbs (trigger finger/thumb), or De Quervain’s tenosynovitis, carpal tunnel syndrome, Dupuytren’s contracture and diabetic stiff hand syndrome.
How physiotherapy can help you?
Exercise is an important factor in the management of diabetes. According to a Harvard Health Publishing article, the importance of exercise when you have diabetes, a carefully designed exercise program helps diabetic patients lower their HbA1c (average blood glucose levels for past 2-3 months) by about 0.7 percent.
According to Harvard Health, benefits of exercise for those with diabetes may include:
Improves ability to control weight
Lowers blood pressure
Lowers harmful cholesterol and raised healthy cholesterol
Strengthens muscle and bones
Reduces anxiety
Lowers blood glucose levels
Raises body’s sensitivity to insulin, helping to overcome insulin resistance
The general guidelines for exercise from the ADA are as follows:
| Aerobic exercise: At least 150 minutes/week of moderate to vigorous exercise Daily exercise is suggested to maximize insulin action Shorter durations (at least 75 minutes/week) of vigorous-intensity or interval training may be sufficient for younger and more physically fit patients May be performed continuously, or as high-intensity interval training |
| Resistance exercise: Progressive moderate to vigorous resistance training should be completed 2 to 3 times/week on nonconsecutive days At least 8 to 10 exercises, with completion of 1 to 3 sets of 10 to 15 repetitions |
| Flexibility and balance training are recommended 2 to 3 times/week for older adults |
| Structured lifestyle interventions that include at least 150 min/week of physical activity and dietary changes resulting in weight loss of 5%–7% are recommended to prevent or delay the onset of type 2 diabetes in populations at high risk and with prediabetes. |
Foot care, Diabetic patients must be aware how to prevent foot problems before they happen. Treatment for diabetic foot problems have recently improved, but prevention remains the best way to prevent complications. Diabetic patients need to learn how to properly examine their own feet and be able to recognize early signs and symptoms of diabetic foot problems.
Tips for Healthy Feet:
Check your feet every day for cuts, redness, swelling, sores, blisters, corns, calluses, or any other change to the skin or nails. Use a mirror if you can’t see the bottom of your feet, or ask a family member to help.
Wash your feet every day in warm (not hot) water. Don’t soak your feet. Dry your feet completely and apply lotion to the top and bottom—but not between your toes, which could lead to infection.
Never go barefoot. Always wear shoes and socks or slippers, even inside, to avoid injury. Check that there aren’t any pebbles or other objects inside your shoes and that the lining is smooth.
Wear shoes that fit well. Diabetics should be educated on proper footwear. Always wear socks with your shoes.
Trim your toenails straight across and gently smooth any sharp edges with a nail file.
Don’t remove corns or calluses yourself, and especially don’t use over-the-counter products to remove them—they could burn your skin.
Get your feet checked at every health care visit
Keep the blood flowing. Put your feet up when you’re sitting, and wiggle your toes for a few minutes several times throughout the day.
Choose feet-friendly activities like walking, riding a bike, or swimming fig – shoes for diabetic patients.
Author
-

BPT, MPT (Musculoskeletal)
View all posts
Assistant Professor
Maharaja Agrasen College of Physiotherapy